That sudden, stabbing sensation in your lower back that stops you mid-movement—like when reaching for a toy your toddler dropped or bending to tie your shoe—isn’t just “normal pregnancy discomfort.” Sharp lower back pain strikes 50-70% of expectant mothers, transforming everyday activities into potential pain triggers. One moment you’re fine, the next you’re frozen with a lightning-bolt sensation that makes you question if something’s seriously wrong.
This guide delivers immediate, evidence-based strategies to identify your specific pain trigger and implement targeted relief. You’ll learn why pregnancy creates perfect conditions for these sharp, stabbing sensations, recognize when it’s a medical emergency versus manageable discomfort, and discover trimester-specific techniques that actually work with your changing body. Most importantly, you’ll gain confidence knowing which interventions are safe and effective at every stage of your pregnancy.
Why Pregnancy Creates Lightning-Bolt Back Pain
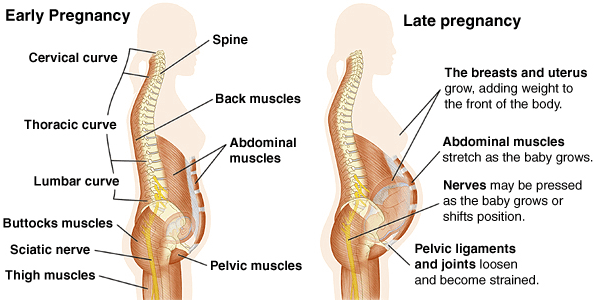
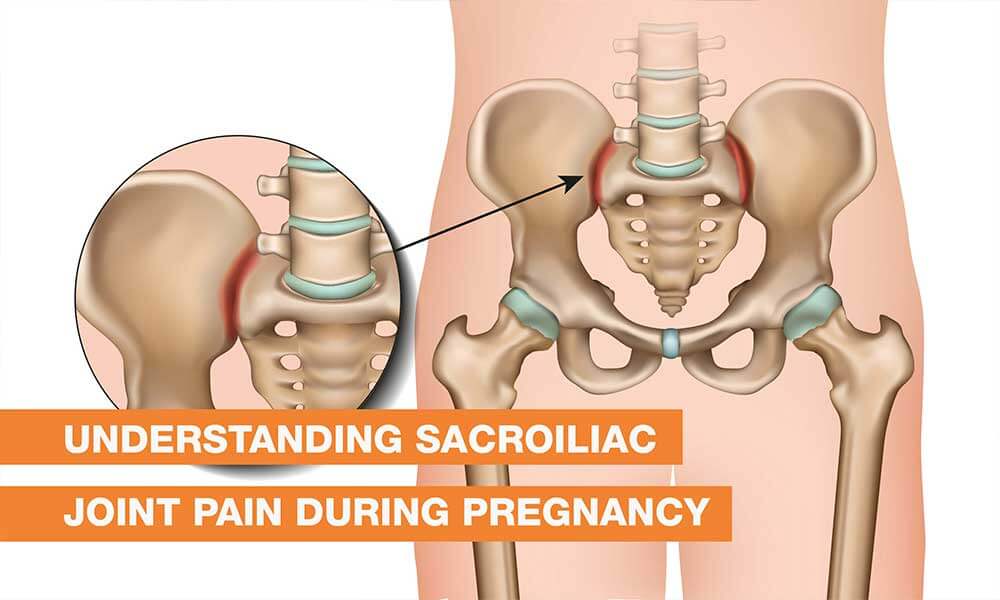
Your body’s remarkable preparation for childbirth inadvertently sets the stage for sharp lower back pain. Relaxin surges to ten times normal levels, intentionally loosening ligaments throughout your pelvis—but this same hormone destabilizes your sacroiliac joints, turning them into wobbly hinges that misfire with simple movements. Imagine trying to walk on a loose door hinge; that’s what your spine experiences with every step you take.
Meanwhile, your center of gravity shifts forward 15-25 degrees as your belly grows, forcing your lower back into an exaggerated arch that compresses facet joints. Add 25-35 pounds of additional weight and separated abdominal muscles losing 30-50% of their stability, and you’ve created the perfect storm where ordinary movements trigger those sudden, sharp pains.
Hormonal Culprits Behind Sudden Stabbing Sensations
Relaxin isn’t working alone—progesterone and estrogen team up to soften all connective tissue, while elevated cortisol increases your inflammation sensitivity. This hormonal cocktail means microscopic joint movements that would normally go unnoticed become interpreted by your brain as severe, localized pain. Your sacroiliac joints, normally stable hinges connecting spine to pelvis, become loose enough that a simple misstep while climbing stairs can feel like a knife in your lower back.
Mechanical Stress Points That Trigger Sharp Pain
Your lumbar facet joints—those small articulations between vertebrae—bear the brunt of your changing posture. As your spine curves forward, these joints jam together, creating sharp, localized pain whenever you extend your back, like standing up straight after sitting. This explains why that simple movement of rising from your office chair can suddenly stop you in your tracks.
Identify Your Specific Pain Trigger Within Minutes
Not all sharp back pain requires the same solution. Pinpointing your exact pain pattern determines which relief strategy will work fastest for your specific situation.
Location-Based Pain Patterns Decoded
Central lumbar pain that worsens when arching backward indicates facet joint irritation. You’ll feel this directly along your spine, often when transitioning from sitting to standing. Relief comes from forward-bending positions and heat therapy.
One-sided sacroiliac pain near your “dimples of Venus” intensifies with weight-bearing activities. This pain typically shoots downward when you stand on the affected leg. Relief involves specific stabilization exercises and SI joint belts.
Deep pelvic sharp pains during walking often signal round ligament stretching. These surprise pains strike mid-stride, then disappear quickly with rest. Gentle stretching and avoiding sudden movements provide relief.
Warning Signs That Demand Immediate Medical Attention
Sharp back pain becomes dangerous when paired with specific symptoms. Seek immediate evaluation if you experience:
- Persistent pain unrelieved by position changes
- Bleeding or fluid leakage
- Fever over 100.4°F or burning urination
- Progressive leg weakness or numbness
- Loss of bladder or bowel control
These combinations can signal preterm labor, infection, or serious nerve compression requiring prompt medical intervention.
Immediate Relief Techniques That Work Within Minutes
When sharp pain strikes, these evidence-based interventions provide rapid relief without medication risks.
Position Reset Protocol for Sudden Pain
Log roll technique transforms bed mobility: lie on your side, bend knees, drop them to one side while rolling your shoulders the opposite direction. This prevents torsion that triggers sacroiliac pain during position changes.
Wall-supported transitions reduce joint stress. When standing from sitting, place hands firmly on armrests or thighs, keep feet wide, and avoid twisting your torso. This simple adjustment prevents the sharp pain that often accompanies standing up.
Heat and Cold Therapy Rules That Actually Work
Heat works best for muscle-related sharp pains. Apply warm compresses for 15-20 minutes to relax spasming muscles and increase blood flow—ideal before activities or stretching.
Cold therapy calms inflammation in joint-related sharp pains. Ice packs for 10-15 minutes reduce swelling in irritated facet joints or sacroiliac areas—apply after activities or when pain feels “hot” and swollen.
Never use heat on areas with numbness or decreased sensation, and avoid cold therapy if you have circulation issues.
Strengthen Your Core Without Risking Diastasis Recti
Traditional abdominal exercises become potentially harmful as pregnancy progresses. Instead, focus on transverse abdominis activation—the deep corset muscle that stabilizes your spine without increasing intra-abdominal pressure.
Daily Stabilization Routine That Prevents Pain
Pelvic tilts form your foundation: 3 sets of 10-15 daily. Lie on your back with knees bent, gently flatten your lower back against the floor by tightening lower abdominal muscles. These teach your brain to engage deep core muscles automatically during daily movements.
Bird-dog progression builds stability without strain. Start on hands and knees, extend opposite arm and leg while maintaining a neutral spine. Hold 5-10 seconds, 10 repetitions. Stop immediately if you feel sharp pain.
Kegel integration creates a natural corset supporting your lower back from below. Contract pelvic floor muscles while exhaling, release while inhaling. Perform 3 sets of 10-15 daily, combining with breathing for maximum benefit.
Sleep Positioning Secrets That Prevent Nighttime Pain
Quality sleep becomes elusive when every position shift triggers sharp pains. Strategic pillow placement creates supported positions that minimize joint stress.
Optimal Side-Lying Setup for Pain-Free Sleep
Left side sleeping improves blood flow while reducing pressure on major blood vessels. Place pillows strategically:
– Between knees to align hips and reduce sacroiliac strain
– Under your belly to prevent ligament stretching
– Behind your back for stability when rolling
– Under your top arm to prevent shoulder collapse
Mattress modifications provide crucial support. A medium-firm surface prevents your hips from sinking too deeply, which twists your spine. If your mattress is too soft, place a board between mattress and box spring for temporary firming.
Workplace Ergonomics That Prevent Pain Buildup
Your office setup can either prevent or provoke sharp back pain throughout the workday. Small adjustments yield significant relief when implemented consistently.
Chair and Desk Modifications That Work
Lumbar support positioning prevents progressive pain buildup. Place a small pillow or rolled towel in your lower back curve, adjusting height so it supports—not pushes—your spine. Replace every 30-60 minutes as your posture changes.
Foot positioning affects pelvic alignment. Use a footrest if your feet don’t touch the ground flat. Keep feet shoulder-width apart and avoid crossing legs, which rotates your pelvis and stresses sacroiliac joints.
Microbreak Protocol for Office Workers
Set phone alarms for 5-10 minute breaks every hour. During breaks:
– Stand and perform gentle pelvic tilts
– Walk to increase circulation
– Do shoulder blade squeezes to counter forward head posture
– Perform ankle circles to prevent swelling
When to Call Your Provider Immediately
Understanding the difference between manageable discomfort and dangerous warning signs prevents unnecessary ER visits while ensuring you never miss critical symptoms.
Emergency Indicators That Can’t Wait
Call your provider immediately if sharp pain comes with:
– Bleeding or fluid leakage
– Regular contractions before 37 weeks
– Fever over 100.4°F
– Severe headache or vision changes
– Decreased fetal movement
Emergency room preparation includes documenting:
– Pain level (1-10 scale) and specific triggers
– Recent activities or possible injury
– Current medications and supplements
– Support person for communication
Postpartum Recovery Timeline You Can Expect
Most women experience significant relief within weeks of delivery, but understanding realistic expectations prevents frustration during recovery.
Immediate Post-Delivery Relief
50% pain reduction typically occurs within 2 weeks as relaxin levels drop dramatically. Many women are surprised by how quickly they feel better—though this varies based on delivery method and individual factors.
Recovery accelerators include:
– Gentle walking starting day 1 (if cleared)
– Proper lifting techniques for your baby
– Gradual return to pre-pregnancy activities
– Continued core strengthening exercises
Long-term Considerations
5-10% of women develop chronic pain requiring ongoing treatment. Risk factors include multiple pregnancies (each increasing baseline risk by 20%) and failure to address muscle imbalances during recovery.
Sharp lower back pain during pregnancy isn’t just “part of the experience”—it’s a manageable condition with specific causes and targeted solutions. By identifying your unique trigger points, implementing evidence-based relief strategies, and knowing when to seek help, you can significantly reduce both frequency and intensity of these debilitating pains. Start with one strategy today—whether it’s adjusting your sleep position or beginning gentle core activation—and build from there. Your body is designed for this remarkable transformation, and with the right tools, you can navigate pregnancy’s physical challenges while maintaining the comfort you deserve.

