That persistent ache between your shoulder blades after hunching over your laptop might seem like just another consequence of desk work. But when thoracic back pain red flags appear, they signal something far more dangerous than poor posture—potentially life-threatening conditions like spinal infections, cancer spread, or heart emergencies. While most mid-back discomfort stems from muscle strain, recognizing these critical warning signs separates routine soreness from medical emergencies requiring immediate action. Ignoring them could mean missing early intervention windows for conditions where hours matter.
These aren’t vague hints your body sends—they’re urgent distress signals demanding your attention. Research confirms that specific symptom clusters dramatically increase the likelihood of serious underlying pathology beyond simple musculoskeletal issues. This guide distills complex medical screening protocols into actionable knowledge you can apply today to protect your spinal health and overall wellbeing.
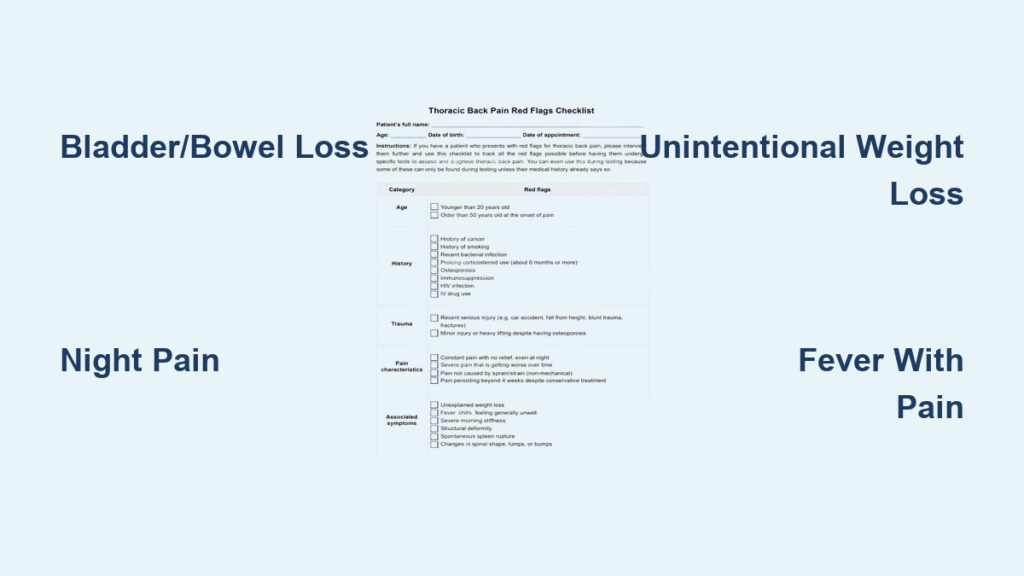
Emergency Neurological Warning Signs You Can’t Ignore
:max_bytes(150000):strip_icc()/spinal-cord-compression-4706467_color-d7ad5f748ada48318e63c1f9e9ca074e.gif)
Bladder or Bowel Dysfunction Requires Immediate Action
Stop everything and call 911 if you experience sudden loss of bladder control, inability to urinate, or unexpected bowel incontinence alongside mid-back pain. These indicate potential spinal cord compression where nerves controlling pelvic functions are compromised. The resource document identifies bladder/bowel dysfunction as a primary neurological red flag requiring urgent imaging. Don’t wait to see if symptoms improve—permanent nerve damage can occur rapidly when these thoracic back pain red flags manifest. Document exactly when symptoms began and whether numbness extends to your inner thighs or groin area.
Progressive Numbness or Radiating Pain Patterns
Watch for numbness spreading from your spine toward your chest, arms, or ribs, especially if it follows a distinct band-like pattern around your torso. Pain radiating to your upper limbs is specifically flagged in research as a critical indicator of nerve compression or serious pathology. Track whether tingling worsens steadily over hours rather than fluctuating with movement. Unlike muscle strain that eases with rest, neurological symptoms often intensify consistently. If you notice progressive loss of sensation combined with mid-back discomfort, seek emergency evaluation immediately—this combination significantly elevates concern levels.
Unexplained Weakness in Limbs
Sudden leg instability, frequent tripping, or hand clumsiness where you drop objects unexpectedly represent urgent neurological warnings. The systematic review explicitly lists neurological signs as primary red flags for serious thoracic conditions. Test yourself by walking heel-to-toe in a straight line—any loss of balance warrants immediate assessment. Similarly, if you struggle with tasks previously manageable (like lifting grocery bags), don’t dismiss it as fatigue. Document whether weakness affects one side more than the other, as asymmetry increases suspicion of spinal cord involvement.
Cancer and Serious Disease Indicators
Night Pain That Disrupts Sleep
Pain severe enough to wake you from sleep—particularly between midnight and 4 AM—is a documented oncological red flag. Unlike mechanical back pain that improves with rest, tumor-related discomfort often intensifies when lying down and may temporarily ease with movement. The research specifically identifies “night pain (pain that awakens patient from sleep)” as a critical indicator requiring investigation. Track whether this occurs repeatedly over several nights, especially if accompanied by unexplained fatigue. Don’t assume it’s just arthritis—this pattern demands medical evaluation to rule out metastatic cancer or primary spinal tumors.
Unintentional Weight Loss with Back Discomfort
Losing weight without dieting or exercise changes while experiencing mid-back pain creates a dangerous red flag combination. The systematic review lists “unintentional weight loss” alongside malignancy history as key cancer indicators. Pay attention if you’ve dropped clothing sizes unexpectedly or notice reduced appetite coinciding with spinal discomfort. This cluster becomes especially concerning when paired with night sweats or persistent fatigue. For individuals over 50 or with cancer history, this triad requires prompt imaging—don’t wait for symptoms to worsen.
Existing Cancer History with New Spinal Pain
Any new thoracic discomfort in patients with prior breast, lung, prostate, kidney, thyroid cancer, lymphoma, or leukemia demands immediate attention. The resource document explicitly flags “malignancy (current or history)” as a primary red flag. Even pain resembling muscle strain requires same-day medical assessment—cancer can metastasize to vertebrae causing structural damage. Contact your oncologist within 24 hours; delays risk permanent neurological damage from spinal cord compression. Never dismiss “just back pain” when cancer history exists.
Infection and Systemic Emergency Signals

Fever Paired with Mid-Back Pain
A temperature over 100.4°F combined with new or worsening thoracic pain signals potential spinal infection. The research identifies “fever” and “recent infection” as critical infection markers requiring urgent intervention. This combination suggests discitis or osteomyelitis—serious spinal infections needing intravenous antibiotics. Don’t treat this as ordinary flu; seek emergency care immediately if you have recent urinary tract, skin, or respiratory infections alongside fever and back discomfort. IV drug users face dramatically elevated risks and require even faster evaluation.
Unexplained Sweating or Breathing Changes
Profuse night sweats (diaphoresis) without environmental cause combined with thoracic pain warrants urgent assessment. The resource lists sweating, dyspnoea (shortness of breath), and haemoptysis (coughing blood) as cardiopulmonary red flags. Pay special attention if breathing difficulties worsen when lying flat or during deep inhalation. These symptoms could indicate pulmonary embolism, aortic dissection, or advanced infections. Unlike musculoskeletal pain that improves with position changes, cardiac or pulmonary-related discomfort often intensifies with respiratory effort.
Trauma and High-Risk Factor Alerts

Minor Falls Causing Disproportionate Pain
Pain developing within 24 hours of even simple falls or twists requires suspicion of vertebral fracture, especially in high-risk groups. The systematic review identifies “history of trauma” as a primary red flag. Osteoporosis patients or those on corticosteroids may fracture vertebrae from minimal force—like sneezing or bending. Document the exact mechanism: “I felt pain after reaching for a coffee cup” provides crucial context. If pain worsens over days instead of improving, seek immediate X-rays; delayed diagnosis risks spinal cord compression.
Corticosteroid Use with New Back Discomfort
Patients taking prednisone or other corticosteroids face dramatically elevated fracture and infection risks with new thoracic pain. The resource explicitly lists “corticosteroids use” as a red flag due to bone density loss and masked infection symptoms. Any mid-back discomfort in steroid users requires imaging—even without obvious trauma. Don’t assume it’s muscle strain; these medications weaken vertebrae while suppressing fever responses that would normally signal infection. Report all steroid use immediately when seeking care.
Documenting Symptoms for Faster Diagnosis
Create a Symptom Timeline Template
Track these critical details for your medical team:
– Exact onset time of pain and associated symptoms
– Pain intensity fluctuations (1-10 scale) throughout the day
– Positional changes that worsen or relieve symptoms
– All associated symptoms as they emerge
This timeline helps doctors distinguish mechanical pain from serious pathology. Note whether pain remains constant regardless of position—a key indicator of non-musculoskeletal causes per the research.
Record Vital Sign Changes
Take and document:
– Temperature every 4 hours during acute episodes
– Resting heart rate when pain peaks
– Blood pressure if you have home monitoring
– Oxygen saturation if you own a pulse oximeter
Fever spikes combined with tachycardia (rapid heartbeat) significantly elevate concern levels per the red flag repository. Bring this log to every medical appointment—it provides objective data often missed in verbal descriptions.
Immediate Action Protocol
When to Bypass Doctors and Call 911
Activate emergency services immediately for:
– Any bladder or bowel control loss
– Saddle area numbness (inner thighs/groin)
– Chest pain with back discomfort
– Sudden leg weakness or walking instability
– Shortness of breath with mid-back pain
These represent the highest-priority thoracic back pain red flags where minutes matter. Don’t drive yourself—paramedics can begin critical interventions en route to the hospital.
Preparing for Medical Evaluation
Before appointments:
– List all medications including dosages and timing
– Note symptom progression with specific time markers
– Bring a companion to advocate and remember details
– Prepare targeted questions about next diagnostic steps
Most importantly: never ignore multiple red flags. Research confirms that single indicators have high false-positive rates, but clusters dramatically increase serious pathology likelihood. If you have fever plus night pain plus weight loss, demand urgent imaging—don’t accept “wait and see” approaches.
Critical takeaway: Thoracic back pain red flags function as your body’s emergency alert system—not subtle suggestions. While isolated symptoms may prove benign, clusters of neurological, oncological, or systemic indicators require immediate medical investigation. Remember that research shows single red flags lack diagnostic precision, but combinations significantly increase the probability of life-threatening conditions. Trust your instincts when symptoms feel “different” from ordinary back strain. Document everything meticulously, prioritize emergency care for neurological or cardiopulmonary warnings, and never dismiss persistent symptoms as “just aging.” Early intervention transforms outcomes for spinal infections, metastatic cancer, and vascular emergencies—making red flag recognition a potentially lifesaving skill. Your spine protects your spinal cord and major organs; when it broadcasts distress signals through these critical indicators, immediate action isn’t optional—it’s essential for preserving your health and mobility.