That persistent ache between your shoulder blades started around week 8, didn’t it? You’re not alone—up to 70% of pregnant women experience upper back pain during early pregnancy, often catching them off guard when they’re still adjusting to their growing belly. What feels like a pulled muscle is actually your body orchestrating an incredible transformation, with hormones surging and your posture shifting to accommodate new life.
This comprehensive guide walks you through exactly why your upper back hurts during these crucial first weeks and delivers practical, safe solutions you can start today. From decoding your pain patterns to proven relief techniques that won’t harm your baby, you’ll discover evidence-based strategies to reclaim comfort during this special time. Most women notice significant improvement within one week of implementing these simple interventions.
Why Upper Back Pain Strikes First Trimester
Your body begins changing immediately after conception, though you won’t notice most shifts until weeks 6-10. The relaxin hormone increases tenfold during pregnancy, loosening every ligament in your thoracic spine. Meanwhile, progesterone peaks at 50-100 times normal levels, causing muscles to relax and reducing spinal support. These hormonal changes combine with physical adaptations that begin surprisingly early.
Postural Shift Timeline
- Weeks 4-6: Minimal changes with occasional tension as your center of gravity begins shifting
- Weeks 7-8: Breast tissue expands 25-50%, pulling shoulders forward and increasing thoracic curvature
- Weeks 9-10: Pectoral muscles tighten from increased breast weight while rhomboids strain to counterbalance
- Weeks 11-12: Peak symptoms as relaxin levels surge and intercostal muscles tense from rib cage expansion
Decoding Your Pain Patterns

Upper back pain during early pregnancy follows predictable patterns once you know what to look for. Most women describe a dull ache between the shoulder blades that worsens throughout the day, often accompanied by burning sensations or sharp stabbing pains when moving suddenly. Recognizing your specific pattern helps target effective relief.
Location Mapping
- Between shoulder blades: Most common site, often bilateral from rhomboid strain
- Base of neck: From compensating for forward head posture and breast weight
- Ribcage wrapping: Intercostal muscle tension from preparing for increased oxygen demands
- Shoulder referral: Pain radiating from pectoral muscle tightness due to expanding breast tissue
Timing Triggers
- Evening worsening: After 8+ hours of postural compensation during daily activities
- Morning stiffness: From sleeping in new positions as stomach sleeping becomes impossible
- Post-meal increase: As diaphragm competes for space with expanding uterus
- End-of-week fatigue: Cumulative muscle strain builds with prolonged sitting or standing
Safe Relief Techniques That Work
Effective treatment focuses on addressing muscle imbalances and postural compensations without medications when possible. These evidence-based interventions provide significant relief for most women within 1-2 weeks of consistent practice.
Daily Stretching Protocol
Morning Routine (5 minutes)
– Cat-camel stretches: 15 reps on hands and knees to mobilize spinal joints
– Shoulder blade squeezes: 10 holds, 5 seconds each to activate rhomboids
– Neck rolls: Gentle circles, 5 each direction to release cervical tension
Evening Routine (10 minutes)
– Wall angels: 2 sets of 10 against wall to improve thoracic mobility
– Pec stretches: Doorway stretch, 30 seconds each side to counter forward shoulder roll
– Chin tucks: 15 reps to counter forward head posture and reduce neck strain
Heat Therapy Guidelines
Apply heat for 15-20 minutes using a heating pad set below 104°F. Moist heat works best—try microwaving a damp towel for 30 seconds. Focus on the rhomboid muscles between your shoulder blades where tension accumulates most. Use heat in the morning to loosen overnight stiffness and again before your evening stretching routine for maximum effectiveness.
Ergonomic Solutions for Daily Life
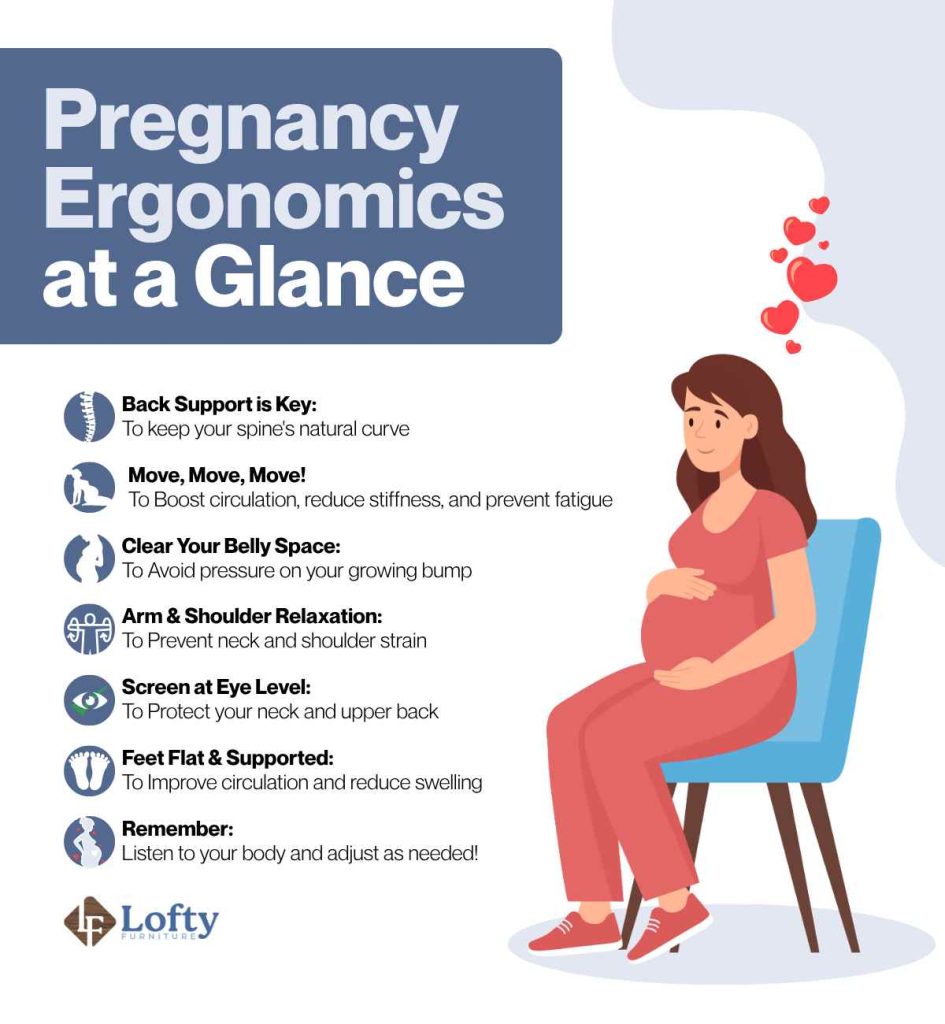
Simple workspace modifications prevent pain from escalating throughout your day. Since 45% of pregnant women report decreased work productivity due to upper back pain, these adjustments prove essential for maintaining professional performance during early pregnancy.
Workstation Optimization
- Monitor height: Top third at eye level to prevent neck strain
- Chair support: Lumbar cushion maintains natural spinal curves
- Keyboard position: Elbows at 90 degrees, wrists neutral
- Micro-breaks: Stand and stretch every 30-45 minutes to prevent muscle fatigue
Sleep Position Strategies
As stomach sleeping becomes impossible, side-lying creates new strain patterns. Use a body pillow between knees and under your belly to maintain spinal alignment. Place a small pillow under your top arm to prevent shoulder roll-forward during sleep. Set phone reminders for hourly position changes during the night to avoid prolonged strain in one position.
When Pain Signals Trouble
While most upper back pain in early pregnancy represents normal musculoskeletal adaptation, certain symptoms warrant immediate medical attention. Understanding these red flags helps distinguish between typical discomfort and potential complications.
Immediate Medical Attention
Seek care within 24 hours if experiencing:
– Severe pain preventing normal daily activities
– Pain accompanied by vaginal bleeding or spotting
– Numbness or weakness extending into arms
– Chest pain or difficulty breathing
– Fever over 100.4°F
Routine Consultation Indicators
Schedule an appointment if:
– Pain persists beyond 2 weeks of consistent home treatment
– Progressive worsening despite interventions
– Sleep disruption lasting more than 3 consecutive nights
– Development of neurological symptoms like tingling
Professional Treatment Options

When home remedies provide insufficient relief, several professional interventions remain safe during the first trimester. These evidence-based treatments show 60-80% improvement rates without medication risks.
Physical Therapy Protocols
Certified prenatal physical therapists address specific muscle imbalances through:
– Manual therapy: Gentle spinal mobilization and soft tissue work
– Postural training: Real-time feedback during daily activities
– Therapeutic exercise: Customized strengthening programs
– Education: Body mechanics for pregnancy and postpartum
Alternative Therapies
- Prenatal massage: Certified therapists use side-lying positions to relieve muscle tension
- Acupuncture: Studies show 60% improvement in pregnancy back pain with minimal sessions
- Chiropractic care: Gentle adjustments by pregnancy-trained practitioners
Prevention Strategies That Last
Implementing preventive measures early prevents 40-60% of upper back pain cases from escalating. These strategies become increasingly important as your pregnancy progresses through the first trimester.
Daily Movement Patterns
- Frequent position changes: Every 30 minutes during prolonged sitting
- Postural awareness checks: Set phone reminders for shoulder blade squeezes
- Proper lifting technique: Bend knees, keep loads close, avoid twisting
- Stair navigation: Lead with stronger leg going up, weaker leg going down
Bra Support Optimization
Professional bra fitting becomes crucial as breast size increases. Most women need 2-3 cup size increases by week 12. Look for:
– Wide, cushioned straps to distribute weight
– Full-coverage cups with no spillage
– Firm band support (shouldn’t ride up)
– Breathable fabrics to prevent skin irritation
Upper back pain during early pregnancy represents your body’s remarkable adaptation to growing new life. While uncomfortable, these symptoms rarely indicate serious problems and respond well to the evidence-based strategies outlined above. Start with the daily stretching protocol and ergonomic modifications today—most women notice improvement within one week of consistent practice.
Remember that every pregnancy differs, and what works for one woman may need adjustment for another. Track your pain patterns, document what provides relief, and maintain open communication with your healthcare provider throughout your pregnancy journey. Understanding your pain timeline helps set realistic expectations—most women experience peak symptoms during weeks 11-13, with 60% reporting significant improvement during the second trimester as their bodies adapt to new postural demands. Continue preventive exercises throughout pregnancy to minimize recurrence and enjoy greater comfort during this special time.